Multimedia Journal of Metaverse in MEDICINE
RESEARCH ARTICLE | JANUARY 2, 2025
A qualitative study on the treatment decision dilemma of elderly patients with digestive tract malignancies
Ruihua Li1, Quncao Yang1, Haonan Wang1, Hao Zhang1, Nan Hao1*
1 Department of Surgical Oncology, The First Affiliated Hospital of Xi’an JiaoTong University, Xi’an 710061, China.
Corresponding Authors: Nan Hao. E-mail: [email protected]
Address: Department of Surgical Oncology, The First Affiliated Hospital of Xi’an JiaoTong University, Xi’an 710061, China.
Abstract
Objective: To explore the dilemma faced by patients over 80 years old and provide scientific basis for improving the quality of treatment decision of patients. Methods: A qualitative research design was used,involving semi-structured interviews with 16 patients over 80 years old and their families. Colaizzi’s seven-step method was used to analyze the data and summarize the themes. Results: The treatment decision dilemmas encountered by elderly patients with digestive tract malignancies includes the lack of independent choice in treatment decisions, insufficient understanding of the disease and decision-making information, inconsistent decision-making within the family, and the conflict between societal pressures and realistic conditions. Conclusion: The treatment decisions of elderly patients with digestive tract malignancies are influenced by a range of factors, including individual, familial, and societal factors. Medical staffs should engage in thorough communication with both patients and their families, conduct comprehensive evaluations of all relevant factors and assist patients and their families to make appropriate treatment decisions in time. This approach will help reduce decisions-making difficulties and improve the quality of decision-making.
Keywords: advanced age; digestive tract malignancy; treatment decision; qualitative study
Introduction
At present, the incidence and mortality rates of malignant tumors in China are above the average level in the world, with digestive tract malignant tumors accounting for about half of these cases[1]. Digestive tract malignant tumors often present insidiously and are often diagnosed in the middle and late stages, by which time the opportunity of radical treatment has been lost. This results in significant physical and psychological suffering for patients[2]. With improvements in living standards and medical advancements, the diagnosis of digestive tract malignancies has increased. The treatment of digestive tract malignant tumors is complicated and diversified, requiring long-term treatment, uncertain prognosis and high treatment costs. In addition, elderly patients generally cannot be financially independent, their self-care ability is decreased, and they are accompanied by many underlying diseases and poor compensatory ability of organ[3]. These factors will affect the patients and their families to make timely treatment decisions. Qualitative research, is a research method in which researchers is a research method in which researchers use multiple data collection methods such as in-depth interview, participatory observation and physical analysis to deeply analyze research objects and reach conclusions[4]. Compared with quantitative research, this method is more in line with humanistic care[5] and can study the real perception of a specific population on a health problem and how patients view the health problem[6]. This study used qualitative research methods to investigate the difficulties in the treatment decision-making process of elderly patients with gastrointestinal malignant tumors and their families, in order to help them improve the quality of decision-making.
Methods
1 Study subjects
Using the method of maximum differentiation and purpose sampling, elderly patients with digestive tract malignancies hospitalized in the oncology department of our hospital from June 2023 to June 2024 were selected as study participants. The sample selection fully considered the different demographic characteristics of the patients. Additionally,the researcher interviewed the primary caregivers and performed parallel participatory observation. Inclusion criteria: A confirmed digestive tract malignancy after pathological examination with no evidence of tumor metastasis; Age≥80 years; Clear cognitive function and intact language ability; Patients is aware of their condition; Voluntarily participation in this interview. Inclusion criteria for family members: Primary caregiver of patients; Clear cognitive function and intact language ability; Involvement in patient treatment and nursing decisions. The study sample size followed the principle of data saturation[7] and the data reached saturation when 16 patients were interviewed in this study.
2 Study Methods
Using phenomenological qualitative research methods, we interviewed and dynamically observed elderly patients with gastrointestinal malignancies and their families to understand the process and dilemma of treatment decision-making.
2.1 Data collection method
(1) Semi-structured interview, in which the researchers introduce the research content, purpose and privacy protection principles to the interviewee in detail, and obtain their informed consent. According to the characteristics of the interviewees and the purpose of the study, the research team made a preliminary draft of the interview including a series of open questions. With reference to the results of the pre-interview with two patients, the official version was revised and sorted out after the initial draft. The main contents of the formal interview were as follows: ①What inner experience did you have after the diagnosis of the disease?② Are there any difficulties in making treatment decisions?③ What are the factors that influence the final treatment decision?④ Do you want to be directly involved in the decision of treatment? In the interviews,the probing and guiding method proposed by Minichiello et al[8] was used to enable interviewees to express their true feelings, but the content and direction of the conversation were not dominated. Interviews were recorded using a voice recorder and field notes. During the interview, we pay attention to listening, encourage the interviewees to tell their true thoughts, and carefully observe and record the the non-verbal behaviors of the interviewees such as body movements, facial expressions and voice characteristics. The duration of each interview was 50-60min, and the interview place was in the oncology surgery talk room, and the interview environment was quiet.
(2) Selectively asking of the patient’s family members
In view of the large proportion of family members involved in the treatment decisions of elderly patients with digestive tract tumors, and the contact with patients for a long time, the situation before and after the disease is relatively understood. Therefore, it is necessary to conduct interviews with family members to fully understand the experience of making treatment decisions for patients.
(3) Participatory observation
In order to avoid over-reliance on the oral narration of the interviewees and grasp the real experience more comprehensively, the researchers made participatory observation in the process of research. There were several oncology nurses in the research team, who carefully observed the patients behavior while doing the treatment and nursing work.
2.2 Data analysis method
In order to ensure the timeliness and accuracy of the data, the arranging of audio files and written materials were completed within 12 hours after the interview[9]. This study followed Colaizzi’s 7-step analysis method[10]. During the analysis, two researchers independently performed continuous and repetitive analysis of each data set. The analysis avoids the inclusion of researchers’ personal subjective experience to ensure the scientific accuracy of the results[11].
2.3 Ethics issues
This study followed the principle of informed consent and signed the informed consent form. All data collected during the process were only used for research purposes. Each interview record was coded in sequence from P 1 to P 16 to protect patients’ privacy.
2.4 Quality control
Both of the two interviewers were oncology nurses, who had frequent contact with the interviewees in daily nursing work, forming a mutual trust and friendly relationship. Meanwhile, a collaborative approach was applied during the research process, ensuring the reliability and validity of the study results. Finally, the collated data were returned to the study participants to check the authenticity of the data.
Results
1 General Information
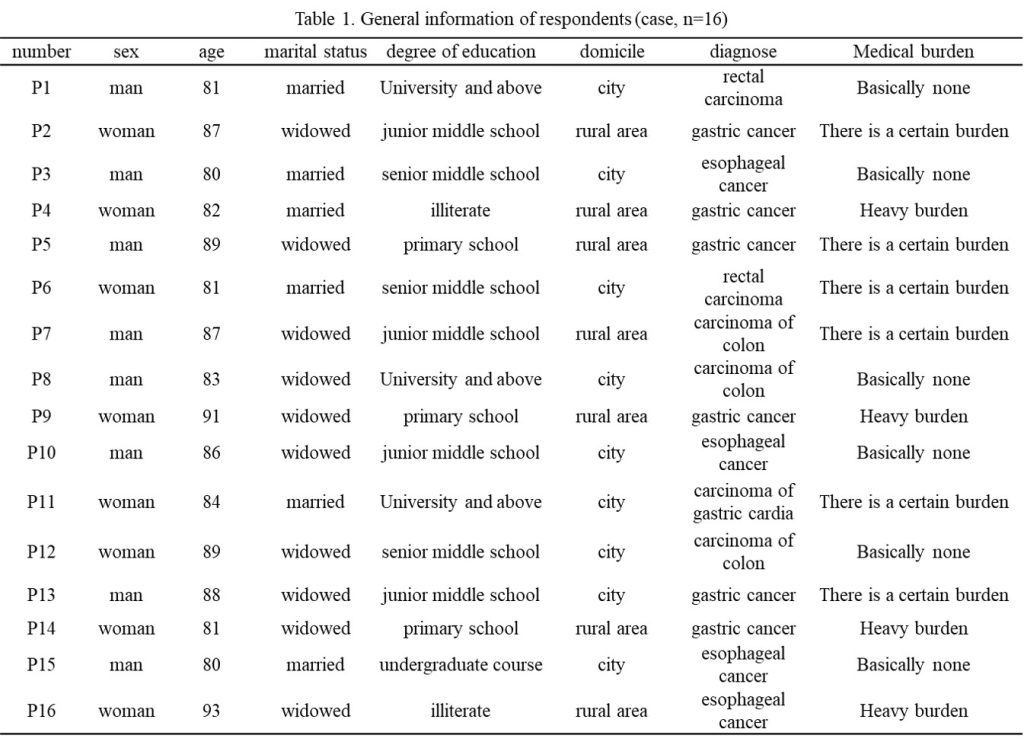
In this study, 16 subjects were interviewed, including 8 males and 8 females, aged 80 – 93 years, with an average age of 85.13 years old. 6 patients were married, 10 were widowed, and all 16 patients had children. Other general information is shown in the table below.
2 Patients lack autonomy in treatment decision-making
Firstly, this is reflected in the concealment of the condition: based on the principle of protective medicine, at the beginning of diagnosis, doctors often withhold the true condition from cancer patients, or they inform the family members and the family decides whether to inform the patient himself. The caregivers of elderly patients with malignant tumors are mostly their children, and they often choose to continue to conceal their illness from patients to avoid causing adverse physical and mental stimulation to patients. As a result, many patients do not learn of their diagnosis until some time after it is confirmed. P1: ” At first, the children told me that it was just an intestinal inflammation, worried that I couldn’t bear it. But nobody lives forever, and besides, I’ve been a doctor all my life, treating and saving, so I don’t feel my life has been in vain.” P5:” At first (family member) told me was gastritis, said it was just a common illness for older people,something easy to treat. Later, when I saw my daughter quietly wiping her tears, I guessed it might be cancer.” P11:” I know I have cancer, I’m aware of my own body.My children thought they could hide it (the diagnosis) from me, but I may be old, but my mind is still clear. The tone and manner of speech from my relatives and friends when they visited were different, and all the other patients in the same ward had cancer. How could I not know I have it too?” Secondly,this is reflected in the passive acceptance of treatment decisions. Cancer patients, especially minors and elderly patients, often lose their autonomy in treatment decision-making, with decisions being made by family members and doctors on their behalf. P1: “I’ve been a doctor all my life, always making treatment decisions for my patients, but now when it’s my turn, I can’t make the decision myself. I wanted to take the risk and preserve my anus, but my children instead advised me to have a colostomy. Now I’ll have to live with a colostomy bag for the rest of my life.” P6: “They didn’t tell me the what was going on and kept asking me to do so many tests—CT scans, colonoscopies, and drew blood several times for tests. I was confused the whole time.” P9:”My children told me I need to have a minor surgery. Do you know how old I am? I’m over 90, I’m practically at death’s door,why bother.” P15: “I’ve always been strong-willed. Although I’m old now, I still want make my own decisions,how to treat my disease and how is the treatment effect. I hope the doctors and my family don’t hide anything from me so I can fully cooperate.”
3 Insufficient information on disease knowledge and decision-making
Firstly, there is a lack of knowledge about the disease. In the early stages of digestive tract tumors, patients often have no obvious discomfort symptoms. Depending on the tumor site, patients may show symptoms such as dysphagia , abdominal distension and pain, changes in bowel habits, weight loss, fatigue and etc. However, these symptoms are often mistaken by patients and family members for indigestion or digestive tract inflammation, leading to the disease is being ignored and treatment decisions are affected. P4: ” At first, I didn’t feeling anything.It was a relative who pointed out that I had lost weight and that said I don’t look as good as before. That’s when I went to the hospital to check.” P8:” No one in our family has ever had cancer, so I never considered that it could be that.I just got some medicine from a local clinic in our hometown, and it worked at first, but later it stopped working. My children insisted that I go to a big hospital for a proper check-up.” P16:” I know cancer is a terminal illness, no matter how much money you spend, it can’t be cured. The children work so hard to earn money, alas, now in my old age, I feel like I’m just burdening them.” Secondly, there is a lack of ability to identify the authenticity of disease treatment information. In today’s highly information-driven society, patients and their families often learn about diseases through the Internet, such as Baidu search and online doctors. These informations are complicated and difficult to distinguish between true and false, which makes patients and their families even more confused when making treatment decisions. P3’s family member: ” I dont know what to do, whether to fight for surgery or opt for conservative treatment. Heard some relatives say there are special drugs that can cure it, while others say if surgery is possible, we should go ahead with it. But my father is so old, and he has diabetes, can he even handle the surgery?” P14’s family member:” I looked up my mom’s symptoms online before, and it seemed like indigestion, so I bought some digestive aids for her. It may have delayed the condition.”
4 Inconsistent decision-making within the family
Due to the uncertainty of prognosis, high treatment costs, and the complexity of cancer treatment,family members often have differing opinions on the treatment. P2’s family member: ” I originally insisted on having surgery for my mother. Although my mother is old, but her health has still been fairly good, and it is possible to have a radical cure after surgery. But my brother did not agree, saying that even with surgery, she might not get better, and the elderly suffer a lot. So, we’re still hesitating..” P7’s family member:” My family situation is special-my grandfather raised me up, I will not give up treatment, but my grandfather has heart disease. My parents are afraid he can not bear such a major surgery, and there may be other complications afterward. I am now struggling with how to choose.” P12’s family member:” The doctor suggested a stoma surgery for my mom, which means she would have to pass stool through an opening in her abdomen and would need to change the stoma bag regularly afterward. I don’t even know how to tell my mother about this.”
5 Conflict between social pressure and realistic conditions
The high cost of treatment, along with societal pressure, significantly influences the decision-making process for patients and their families. P10’s family member: ” the old man is old, and has diabetes and high blood pressure. I’m really afraid that surgery could be risky, and a major surgery would cause a lot of suffering. But if we don’t go ahead with surgery, what will the relatives and neighbors think? They’ll say, ‘You wouldn’t even spend money on your own father, you’re a disgrace,’ and things like that. So now, I really don’t know what to do.” P13’s family member:” A few years ago, my father passed away because of cerebral infarction, and we had to borrow several ten thousands from relatives and friends. We’re still paying off that debt. Now my mother has this illness, alas, I really can’t afford it, but if I give up, I feel like people around me will look down on me.”
Discussion
1 Cultivate a positive doctor-patient relationship and build a doctor-patient shared decision-making model
Treatment decision-making model can be divided into paternalistic, informed, and shared decision-makings. Among these, the shared decision-making model is a treatment plan developed by combining the patient’s own treatment attitude and the medical advice provided by healthcare professionals[12]. This model not only ensures that the patient’s treatment needs are respected but also combine the patients decisions with scientific medical plans[13][14]. Research by Wang Yuan et al[15] found that the shared decision-making model helps improve cancer patients confidence in treatment, alleviate psychological disorders, and improve patient’s treatment adherence and satisfaction. Research by Li Jiaqian et al[16]found that most cancer patients do not want doctors or their families to hide their illness; they prefer to understand their physical conditions, learn the truth about their illness, and exercise their right to be informed. Given that China is a developing country with a large population, unique cultural background and national conditions,informing cancer patients about their diagnosis is not an easy task[17]. However, with the development of medical care and the influence of Western culture, people’s attitudes and perceptions towards cancer have gradually change: neither concealing the true condition of cancer patients nor informing the family members does not fulfill the patient’s right of informed consent[18]. Therefore, healthcare professionals should cultivate a good and harmonious doctor-patient relationship with both patient and their family. It is essential to fully understand the patient and their family’s attitude toward the disease, their need for knowledge about the condition and their demands for treatment, participate in treatment decision-making process and reach an agreement on how to implement treatment[19]。
2 Assist elderly patients and their families in understanding the diseases and improving health literacy
Research has found that comprehensive and objective disease understanding, timely recognition of disease symptoms, early treatment initiation and proactive self-regulation can not only enhance the treatment confidence of cancer patients and their families, but also improve the patient’s quality of life of [20][21][22][23]. When healthcare professionals discuss treatment plans with elderly patients with gastrointestinal malignancies and their families, they should accurately understand the patient’s disease cognition, attitude toward seeking medical care, and expectations regarding treatment outcomes. Additionally, healthcare providers should explain the basic knowledge about the disease, treatment options, treatment recommendations, and prognosis in simple terms. This helps improve the ability of patients and families to distinguish relevant information, enabling them to make better-informed treatment decisions.
3 Use social support system to reduce decision-making dilemmas
Social support is an important factor influencing the medical decision-making behavior of elderly patients[24][25]. Given the complexity of tumors and the uncertainty of prognosis, elderly cancer patients and their families are prone to negative emotions. A well-established social support system can help patients and their families reduce anxiety and fear, gaining more confidence and strength,which enables them to be able to deal with the disease more positively. Social support is the most potential resource for cancer patients and their families when facing illness. A good social support system should include comprehensive support from healthcare professionals, family members and social networks. During hospitalization, healthcare providers should not only offer medical support but also listen to the emotional needs of the patient, providing emotional, evaluative, and informational support. As one of the behavioral intervention methods for cancer patients. Peer support, as one of the behavioral interventions of cancer patients, plays an important role in guiding positive thinking of patients and their families. Establishing patient support groups can help patients and their families make timely treatment decisions and build confidence in the treatment process. Since cancer treatment is often costly, many places have carried out social poverty alleviation actions for poor cancer patients, providing assistance and resources to poor families, which greatly reducing their economic burden.
Conclusion
In China, the current situation of medical decision-making in elderly patients with digestive tract malignancies is that patients often lack the autonomy in treatment decision and even the right to be informed about their condition. Instead, decisions are usually made by family members, particularly their children. often replace the decision-making. Due to the insufficient knowledge about the disease and decision-making information, patients often unable to recognize the correlation between their own discomfort and tumor in a timely manner, and thus, leading to delays in diagnosis and treatment. Faced with a large volume of complex and conflicting information about the disease , patients and their families often fall into a dilemma when making treatment decisions. It is also difficult to quickly agree treatment opinions within family members. Furthermore, treatment decisions are influenced by economic factors and societal pressures. Therefore, effective measures should be taken to reduce decision-making dilemmas on the basis of building a good and harmonious doctor-patient relationship and making full use of social support. Healthcare providers should help patients and their families to understand the disease and improve the level of health literacy. Through collaboration between healthcare professionals, patients, and their families, the best treatment decisions should be made in a time.
Author Contributions
Ruihua Li wrote the first draft. Quncao Yang, Haonan Wang and Hao Zhang contributed to the critical revision of the manuscript. Nan Hao reviewed and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
None.
Conflicts of Interest
The authors declare no conflict of interest.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Received: 10 November 2024
Accepted: 17 December 2024
Published on line: 2 January 2025
Reference
- Liang CL, Yang WS. Clinical Analysis of Malignant Tumors of the Digestive Tract. Medical Information, 2019, 32(18): 124-125+128.
- Chen BY. Clinical significance of serum CRP and tumor markers detection in digestive tract malignancy. International Infectious (electronic), 2020,9(02):107.
- Chen DQ, Li BX, Meng L. Effect of ulinastatin on laparoscopic perioperative liver function in elderly patients with gastrointestinal malignancies. The Northwest Journal of Pharmacy, 2017, 32(02):212-214.
- David Hughes, Tian N, Wu QF. Application of qualitative methods in health policy and management research. Medicine and Society, 2021,34(01):1-9.
- Cheng L, Feng S, Lu CM, et al. Systematic evaluation and Meta integration of the qualitative study of parental care experiences after premature infant discharge. The Chinese Journal of Evidence-based Medicine, 2015, 15(09):1090-1097.
- Zhao R, Zheng G, Huang CF, et al. The application value of the systematic evaluation of qualitative research in the development of evidence-based guidelines. Chinese Journal of Evidence-based Medicine, 2016,16(07):855-859.
- He J, Jiang WL. A qualitative study of the burden experience of family caregivers in patients with chronic heart failure. PLA Journal of Nursing, 2016,33 (1):26-28,43.
- Minichiello V, Aroni R, Timewell, Alexander L. In.Depth Interviewing. Melbourne Longman, 1995: 138-152.
- Wang BH, Yan XY, Zhu Q. Quality study of inpatient participation in medication safety awareness. Nursing Research, 2017, 31 (27): 3448-3451.
- Northall T, Chang E, Hatcher D, et al. The application and tailoring of Colaizzis phenomenological approach to a hospital setting. Nurse Researcher, 2020, 28(2).
- Hao N, Sun YL, Zhang H. A qualitative study of the spiritual needs of young patients with gastric cancer. Chinese Medical Ethics, 2018,31(06):717-721.
- Yao SY, Zhang W, Luo YH, et al. Progress in research on doctor-patient joint decision-making. China Nursing Management, 2017,17(03):428-431.
- Truglio-Londrigan M, Slyer JT. Shared decision-making for nursing practice: an integrative review. Open Nurs J, 2018, 12:1-14.
- Blanc X, Collet TH, Auer R, et al. Publication trends of shared decision making in 15high impact medical journals: a full-text review with bibliometric analysis. BMC Med Inform Decis Mak, 2014, 14:71.
- Wang Y, Li SY, Gu Y. Participation in doctor-patient decision-making among doctor-patients operated on malignant tumors. Clinical and Rehabilitation of Oncology in China, 2019,26(06):743-746.
- Li JQ, Wu T, Yan L. A qualitative study of real disease information and treatment decision preference in cancer patients of different gender. Evidence-based care, 2019, 5(10): 907- 910.
- Yue L, Pang W. Progress in the cognition of informed consent to cancer and the exploration of the informed model of cancer. Tianjin Nursing, 2018,26(05):621-623.
- Tu J, Mei smiled. Patient “autonomy” reconsideration —— based on the disease notification practice study of cancer patients in G City Z Hospital. Journal of Southeast University, 2019,21(5):96-104.
- Aaron C, Chiarello LA, Palisano RJ, et al. Relationships among family participation, team support, and intensity of early intervention services. Phys Occup Ther Pediatr, 2014, 34(4): 343-355.
- Huang Qi. Preliminary study of disease perception and post-traumatic growth in lung cancer patients. Anhui Medical University, 2019.
- Fisher A, Manicavasagar V, Sharpe L, et al. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health,2018,27(1):66-79.
- Paschal AM, Mitchell QP, Wilroy JD, et al. Parent health literacy and adherence-related outcomes in children with epilepsy. Epilepsy Behav,2016,56:73-82.
- Jin M, Wang WL, Pan Q, et al. The mediating role of coping methods between hope and psychological distress in patients with gastric cancer chemotherapy. Chinese Journal of Practical Nursing, 2015,31(14):1023-1027.
- Zhang YX, Feng W. Application of decision tree in the influencing factors of poor rural elderly care. Journal of Peking University (Medical edition), 2018,50 (03): 450-456.
- Pan HZ, Wang QQ, Qin YH, et al. Analysis of health service status and influencing factors for the rural poor population in Guangxi. Modern Hospital Management, 2015,13 (03): 20-23
