Multimedia Journal of Metaverse in MEDICINE
RESEARCH ARTICLE | JANUARY 2, 2025
Analysis of the Application Effect of the Enhanced Recovery After Surgery (ERAS) Concept in Perioperative Nursing for ERCP Treatment of Biliary Stones
Ning Zhao1, Sha Peng1, Zhengwei Wang1, Hao Zhang1, Yong Zhang1*
1 Department of Surgical Oncology, The First Affiliated Hospital of Xi’an JiaoTong University, Xi’an 710061, China.
Corresponding Authors: Yong Zhang. E-mail: [email protected]
Address: Department of Surgical Oncology, The First Affiliated Hospital of Xi’an JiaoTong University, Xi’an 710061, China.
Abstract
Objective: To compare the safety and clinical value of enhanced recovery after surgery (ERAS) and conventional management in the treatment of common bile duct stones with ERCP. Methods: The clinical data of 62 patients who underwent ERCP from May 2014 to May 2017 in Hefei Second People Hospital were analyzed retrospectively. Among them, there were 31 cases of perioperative management with ERAS(ERAS group, n=31) , 31 cases were treated by conventional management (conventional group, n=31). Two group were compared the incidence of intraoperative blood loss, the first time of feeding, the incidence of postoperative complications(such as nausea, vomiting, abdominal pain, hemorrhage, pancreatitis, cholangitis), cholangiography and indwelling time, length of stay, Differences in hospitalization costs. Results: Compared with the traditional group, ERAS group had 32.00 ± 18.33h for the first time after eating, 45.6 ± 30.344h in the traditional group, 26.53 ± 7.431h in the nasal cholangiopancreatography and the retention time in the ERAS group, the traditional group was 375.66 ± 19.910h, the hospitalization time ERAS group 10.23 ± 2.771h, the traditional group was 16.29 ± 6.323h, which was significantly shorter than that of the traditional group (P <0.05). The intraoperative hemorrhage ERAS group was 2.65 ± 1.631ml and the postoperative complication ERAS group 3 (5.3) was significantly less than that of the traditional Group, hospitalization costs ERAS group 28981.77 ± 6478.062, compared with the traditional group was also significantly reduced (P <0.05). Conclusion: The concept of accelerated rehabilitation surgery is a safe, economical and effective method for the treatment of biliary calculi with ERCP.
Keywords: rapid rehabilitation surgery; biliary calculus; retrograde cholangiopancreatography; postoperative complications
Introduction
In recent years, with changes in dietary habits and lifestyle, the incidence of liver and gallbladder diseases has increased year by year. Surgery is a common treatment method, but some patients are prone to various complications after surgery. Therefore, nursing interventions during surgery are particularly important. Enhanced Recovery After Surgery (ERAS) uses a series of evidence-based perioperative measures to reduce physiological and psychological stress caused by surgery and medical procedures. By providing multidimensional, comprehensive care combined with surgical and anesthesia techniques, ERAS aims to reduce postoperative complications and enable rapid recovery. It challenges the traditional perioperative care principles that have been in place for nearly a century. Research has shown that ERAS has significant advantages over traditional methods in terms of shortening hospital stay, reducing postoperative complications, mortality, and medical costs. Currently, ERAS concepts and practices are widely applied in minimally invasive surgery, but there are no unified standards or evaluations for their use in endoscopic retrograde cholangiopancreatography (ERCP) surgery. Therefore, we conducted a retrospective analysis of patients who underwent ERCP surgery at our hospital from January 2017 to December 2019 using the ERAS concept in nursing interventions to explore its effect on perioperative care for biliary stone treatment.
Methods
We selected 62 patients who underwent ERCP surgery at our hospital between January 2017 and December 2019 as study subjects. Based on the nursing approach, the patients were divided into two groups: the experimental group (31 patients), who received ERAS-based perioperative care, and the control group (31 patients), who received conventional care. All patients met the following inclusion and exclusion criteria:
Inclusion criteria:
1. All patients were diagnosed with common bile duct stones combined with gallbladder stones through imaging techniques such as CT and MRI;
2. No severe cardiopulmonary complications, ASA classification I or II;
3. No history of upper gastrointestinal surgery;
4. Complete clinical data and signed informed consent.
Exclusion criteria:
1. Common bile duct stones larger than 2.5 cm in diameter;
2. Clear bile duct stricture or malformation;
3. Patients with malignant tumors or coagulopathy;
4. Mental disorders preventing cooperation.
The control group received conventional perioperative nursing, mainly including monitoring of the condition, medication guidance, etc.
The experimental group received perioperative nursing interventions based on the ERAS concept, with specific measures as follows:
(1) Preoperative Nursing:
a. Psychological Care: Patients often have negative perceptions of their condition and lack understanding, leading to varying degrees of anxiety and depression. Timely psychological counseling was provided, along with ERAS-related education to improve patient cooperation.
b. Preoperative Preparation: On the night before surgery, patients were given 1000 mL of 10% glucose solution, and on the morning of surgery, 500 mL of 10% glucose solution. Patients were instructed to fast for 4-6 hours before surgery and refrain from drinking for 2 hours, while also receiving bowel care to prevent intra-abdominal infection during surgery.
(2) Intraoperative Nursing:
The patient’s position was adjusted, and appropriate temperature and humidity were set before and during surgery. Measures were taken to maintain warmth and manage the nasobiliary tube and catheter to prevent infection and abdominal distension.
(3) Postoperative Nursing:
a. Encouraging the patient to get out of bed 6 hours after surgery, with pain management based on pain scores.
b. If there was no obvious biliary infection, antibiotics were given 30 minutes before surgery and stopped 24 hours postoperatively.
c. A cholangiogram was performed 24 hours after surgery, with the tube removed the following day.
d. Fluid intake was controlled at 2000 mL within the physiological requirement, with an infusion rate of 250 mL/h. Additionally, dietary and rehabilitation training guidance was provided.
Evaluation Indicators
a. Clinical indicators such as intraoperative blood loss, time of first flatus, first defecation, time of first out-of-bed activity, first meal, nasobiliary tube placement, hospital stay, and hospital costs were recorded.
b. Complications such as postoperative white blood cell count, serum amylase, cholangitis, pancreatitis, and bleeding were observed within 24 hours post-surgery.
Statistical Methods
Continuous variables were expressed as mean ± standard deviation, and categorical variables as percentages. The t-test was used to compare differences in continuous variables between the experimental and control groups, while the Chi-square test or Fisher’s test was used to compare categorical variables. Statistical analyses were performed using SPSS version 24 (Chicago, IL, USA), with a two-sided P value < 0.05 considered statistically significant.
Results
Basic Patient Information
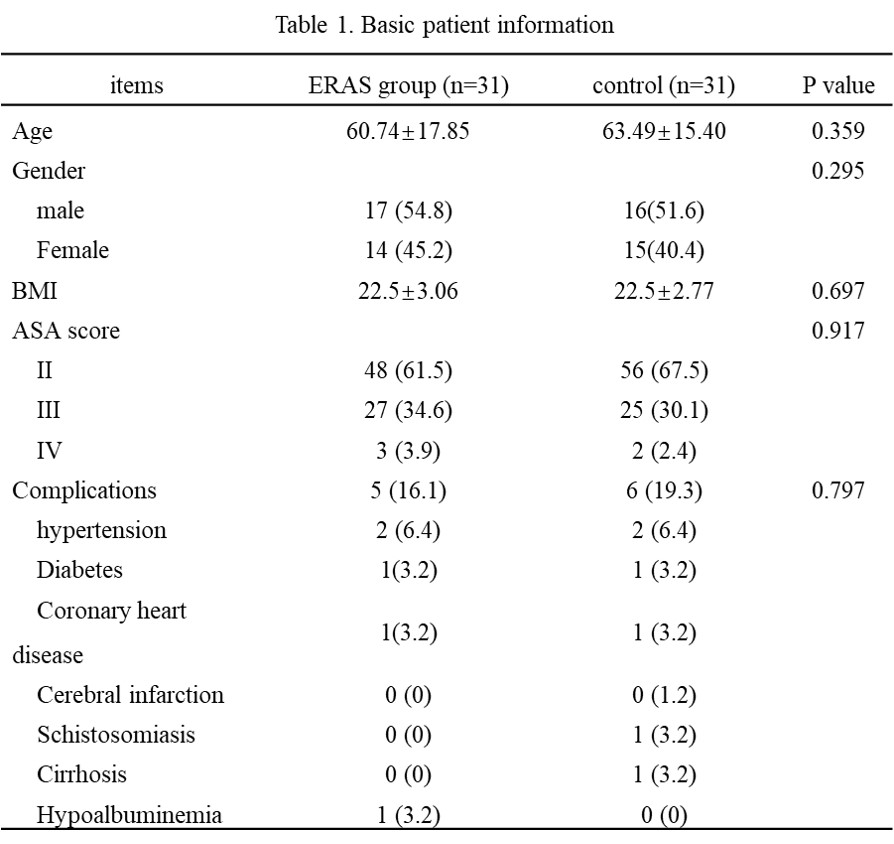
The demographic data of all patients included in the study are shown in Table 1. There were no statistically significant differences between the experimental and control groups in terms of age, gender, or BMI (Table 1).
Comparison of Clinical Indicators Between the Two Groups
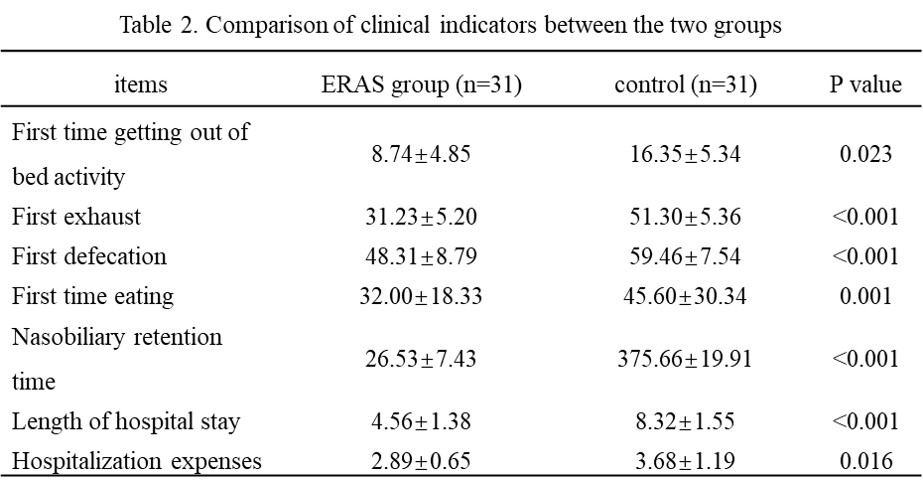
The experimental group had significantly shorter times for first meals, nasobiliary tube placement and removal, hospital stay, and other indicators compared to the control group, with statistically significant differences (P < 0.05) as shown in Table 2.
Comparison of Intraoperative Blood Loss and Postoperative Complications Between the Two Groups
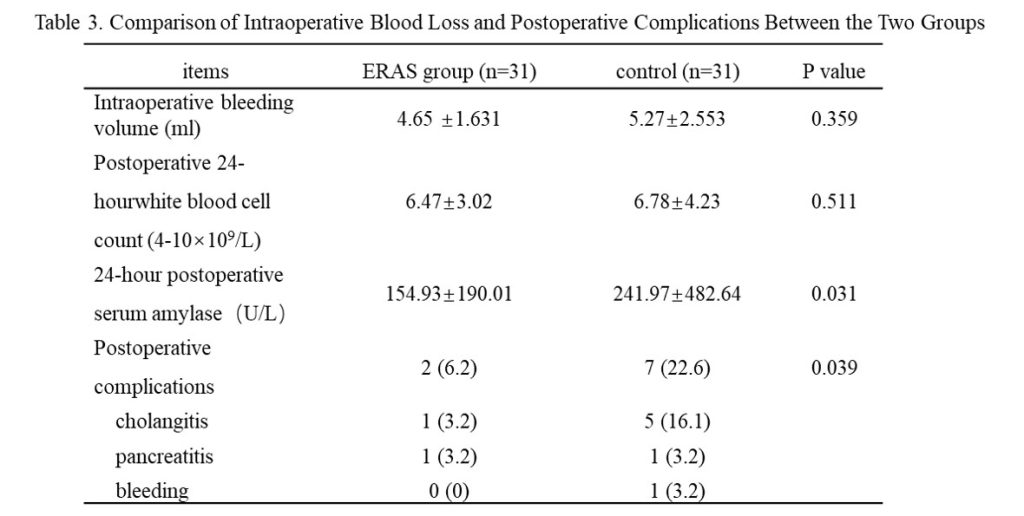
The experimental group had significantly less intraoperative blood loss, fewer postoperative complications, and lower serum amylase levels 24 hours post-surgery than the control group (P < 0.05). There were no significant differences in postoperative white blood cell levels between the two groups (P > 0.05), as shown in Table 3.
Discussion
Enhanced Recovery After Surgery (ERAS), proposed by Kehlet in 1997, is a new perioperative management concept that aims to reduce the negative physiological and psychological stress caused by surgery and medical procedures through a series of evidence-based perioperative optimization measures. This approach helps minimize negative responses and accelerates recovery. The concept was later reintroduced and implemented by Danish surgeons Wilmore and Kehlet in 2001. Currently, ERAS is widely applied in colorectal, orthopedic, gynecologic, gastric cancer, and cardiothoracic surgeries, with evidence supporting its clinical effectiveness. However, there are relatively few studies on the clinical application of ERAS in biliary surgery, especially in ERCP + EST for biliary stone treatment.
In this study, we retrospectively analyzed the clinical data of patients treated with ERCP + EST for biliary diseases at our center, aiming to evaluate the safety and clinical value of applying the ERAS concept in this context.
Our analysis included ERAS-based measures such as psychological care and ERAS education before surgery, nonsteroidal anti-inflammatory drugs after surgery to reduce inflammation, and encouraging early mobilization to promote recovery. We observed that patients in the ERAS group had shorter hospital stays, fewer complications, and lower hospital costs compared to the control group, confirming the safety and economic benefits of ERAS in ERCP + EST treatment.
However, this study has some limitations. It is a retrospective study based on a database, lacking randomization, and the differences in perioperative care may affect recovery outcomes. Moreover, as different nurses were involved in the care, and there were no standardized treatment protocols, this could introduce bias. Additionally, due to limited follow-up, we cannot determine the long-term survival impact of different perioperative nursing methods. Despite these limitations, the study provides valuable data for improving the safety and effectiveness of recovery after ERCP treatment for biliary stones.
Conclusion
The ERAS concept applied to the perioperative nursing of ERCP treatment for biliary stones is safe and effective. It not only accelerates patient recovery but also reduces complications, making it worthy of promotion in clinical nursing practice.
Author Contributions
Ning Zhao wrote the first draft. Sha Peng and Zhengwei Wang contributed to the critical revision of the manuscript. Hao Zhang and Yong Zhang reviewed and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
None.
Conflicts of Interest
The authors declare no conflict of interest.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Received: 22 October 2024
Accepted: 12 December 2024
Published on line: 2 January 2025
Reference
- Kehlet H, Wilmore D W. Ann Surg(Annals of surgery), 2008, 248(2):189-198.
- Bosio R M, Smith B M, Aybar P S, Senagore A J. Am J Surg(American journal of surgery), 2007, 193(3):413-415, 415-416.
- Wilmore D W. Ann Surg(Annals of surgery), 2002, 236(5): 643-648.
- Kehlet H, Wilmore D W. Am J Surg(American journal of surgery), 2002, 183(6):630-641.
- Li H, Liu Y, Li Q, Fan J, Gan L, Wang Y. Eur Geriatr Med(European geriatric medicine), 2020.
- Steenhagen E. Nutr Clin Pract(Nutrition in clinical practice : official publication of the American Society for Parenteral and Enteral Nutrition), 2016, 31(1):18-29.
- Xu E X. Ann Transl Med(Annals of translational medicine), 2015, 3(9):129.
- Carron M, Ieppariello G, Safaee F B, Foletto M. Br J Surg(The British journal of surgery), 2020, 107(6):772-773.
- Pedziwiatr M, Pisarska M, Kisielewski M, Major P, Mydlowska A, Rubinkiewicz M, Winiarski M, Budzynski A. Med Oncol(Medical oncology (Northwood, London, England)), 2016, 33(6):56.
- Pedziwiatr M, Pisarska M, Kisielewski M, Matlok M, Major P, Wierdak M, Budzynski A, Ljungqvist O. Med Oncol(Medical oncology (Northwood, London, England)), 2016, 33(3):25.
- Tiefenthal M, Asklid D, Hjern F, Matthiessen P, Gustafsson U O. Colorectal Dis(Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland), 2016, 18(2):187-194.
- Vlug M S, Wind J, Hollmann M W, Ubbink D T, Cense H A, Engel A F, Gerhards M F, van Wagensveld B A, van der Zaag E S, van Geloven A A, Sprangers M A, Cuesta M A, Bemelman W A. Ann Surg (Annals of surgery), 2011, 254(6):868-875.
- Pedziwiatr M, Pisarska M, Kisielewski M, Major P, Matlok M, Wierdak M, Natkaniec M, Budzynski A. World J Surg Oncol(World journal of surgical oncology), 2015, 13:330.
- Ota H, Ikenaga M, Hasegawa J, Murata K, Miyake Y, Mizushima T, Hata T, Takemasa I, Yamamoto H, Sekimoto M, Nezu R, Doki Y, Mori M. Surg Today(Surgery today), 2017, 47(6):668-675.
- Li J, Kong X X, Zhou J J, Song Y M, Huang X F, Li G H, Ying X J, Dai X Y, Lu M, Jiang K, Fu D L, Li X L, He J J, Wang J W, Sun L F, Xu D, Xu J Y, Chen M, Tian Y, Li J S, Yan M, Yuan Y, Ding K F. BMC Cancer(BMC cancer), 2019, 19(1):988.
- Hur H, Roh C K, Son S Y, Han S U. J Surg Oncol(Journal of surgical oncology), 2020.
- Moggia E, Koti R, Belgaumkar A P, Fazio F, Pereira S P, Davidson B R, Gurusamy K S. Cochrane Database Syst Rev(The Cochrane database of systematic reviews), 2017, 4:D11384.
- Yildirim A E, Ozturk Z A, Konduk B T, Balkan A, Edizer B, Gulsen M T, Savas M C, Kadayifci A. Acta Gastroenterol Belg(Acta gastro-enterologica Belgica), 2017, 80(2):263-270.
- Yang J, Wang W, Liu C, Zhao Y, Ren M, He S. J Clin Gastroenterol(Journal of clinical gastroenterology), 2020, 54(4):305-313.
- Nawaz M H, Sarwar S, Nadeem M A. Pak J Med Sci(Pakistan journal of medical sciences), 2020, 36(3):426-431.
- Mu P, Yue P, Li F, Lin Y, Liu Y, Meng W, Zhou W, Li X. Turk J Gastroenterol(The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology), 2020, 31(3):193-204.
- Kang X, Zheng L, Zeng W, Yang S, Sun H, Zhang R, Wang X, Wang B, Tao Q, Yao S, Chen J, Pan Y, Guo X. J Gastrointest Surg(Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract), 2018, 22(11):1903-1910.
- Hakuta R, Kawahata S, Kogure H, Nakai Y, Saito K, Saito T, Hamada T, Takahara N, Uchino R, Mizuno S, Tsujino T, Tada M, Sakamoto N, Isayama H, Koike K. Dig Endosc(Digestive endoscopy : official journal of the Japan Gastroenterological Endoscopy Society), 2019, 31(1):59-68.
- Hung T H, Tseng C W, Chen Y C, Tseng K C, Hsieh Y H, Tsai C C. Medicine (Baltimore)(Medicine), 2019, 98(30):e16529.
- Zhang W, Che X. World J Surg Oncol(World journal of surgical oncology), 2020, 18(1):71.
